Previous Pregnancy Loss
Treatments
- Endometrial Receptivity Array
- Fertility Surgery
- Microbiome Investigation
- PGD
- PGS
- Blastocyst Transfer
- Sperm DNA Fragmentation
- IVF
- Uterine nk Cells Detections
- Autoimmune Diseases
- Karyotyping
- Fertility Booster Diet
- Weight Loss Management
- Immunotherapy for Pregnancy
Endometrial Receptivity Array
What is it?
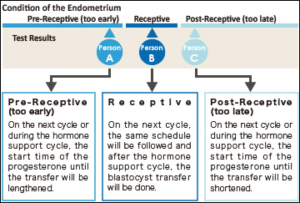 The term ERA stands for Endometrial Receptivity Analysis or Array. In this test, a small sample tissue from endometrial lining (innermost layer of Uterus) is used for evaluating whether the Uterus is ready for implantation of embryo or not.
The term ERA stands for Endometrial Receptivity Analysis or Array. In this test, a small sample tissue from endometrial lining (innermost layer of Uterus) is used for evaluating whether the Uterus is ready for implantation of embryo or not.
In the menstrual cycle of a woman the period from 19th to 23rd days is known as “implantation window” during which, the uterus gets prepared for the implantation process. It is part of the luteal phase and the endocrine part of ovaries is producing progesterone. This progesterone brings about modifications in the uterine wall so that, it gets prepared for receiving the embryo. The process involves formation of certain proteins that make the lining thicker and more receptive. In majority of females (84%) this window occurs at the exact time while in very few females (16%) this window occurs either before or after this period.
The IVF treatment in such cases fails as, the embryo transfer is occurring at wrong time. It is happening at the time, when the implantation window is either yet to open or has already been closed. So, the implantation is failing.
When is it prescribed?
It is prescribed in the patients where recurrent implantation failures are observed.
How is it done?
- A small endometrial tissue is collected and expression level of the gene 238 which determines endometrial receptivity is investigated.
- The technique involves assessing RNA levels in different stages of menstrual cycle. As this test is reproducible, its findings remain the same months after and hence, the test is not required to be repeated.
- This investigation can clearly indicate whether this implantation window of a particular woman is happening at the right time or the embryo transfer needs to be scheduled on the different date to match the window so that maturation of endometrial lining can be synchronized with embryo.
What are the advantages?
- Due to precise identification of Implantation Window, embryo transfer can be appropriately planned and can yield assured results.
- The agony of failed transfer can be got rid of.
- A minor shift by one of two days in embryo transfer can result into pregnancy.
Fertility Surgery
What is it?
A corrective surgery advised for the patients having structural abnormality of reproductive organs so as to improve the chances of conception. It can be for the male or the female partner.
How is it done?
First, minimal invasive diagnostic techniques are used to identify the problem and then a suitable surgical procedure is performed to correct it. The protocol can shortly shown as follows :
Female:
- Reversal of Tubectomy (Tubal ligation). The patient who has already undergone tubectomy for avoiding further pregnancies if decides to have a baby, this kind of surgery can be a solution wherein the ligatured (closed) fallopian tube is reconnected.
- Reconnecting fallopian tube: If there is blockage in fallopian tube due to some infection and pregnancy is not happening because of this, the tube can be reconnected surgically to solve the problem. It involves insertion of a small tube through cervix, uterus and connect the fallopian tube. The surgery is called Salpingostomy, sometimes called neosalpingostomy (the fallopian tube may be cut completely to open the passage for egg cells) or fimbrioplasty (when the tip of fallopian tube that is very close to ovarian is blocked, the tip if surgically opened).
- Polypectomy: A polyp is an abnormal collection of tissue. A polypectomy is a surgical procedure to remove polyps from the from an organ like Uterus. The procedure is relatively noninvasive and is usually carried out at the same time as a hysteroscopy.
- Myomectomy: This procedure sometimes also known as fibroidectomy, refers to surgical removal of uterinefibroids (leiomyomas). In comparison to hysterectomy, the uterus remains preserved in this procedure and the woman retains her reproductive potential.
- Dilatation for treating cervical stenosis: Cervical stenosis means a conditions wherein the cervix becomes extremely narrow. The treatment for this condition is using a dilator.
- Adhesiolysis: Some times, pelvic adhesions are observed blocking passage between uterus and ovarian. In such conditions natural pregnancy becomes difficult and even in ART oocyte pickup is obstructed by the adhesions. This disorder is treated by microsurgical technique or laparoscopic surgery to remove the adhesion and prevent its recurrence.
- Metroplasty: Sometimes, uterus is abnormal in shape such as ‘T’ or heart shaped and hence, can lead to complications during and after pregnancy. This condition is treated with metroplasty. The surgery involves reconstruction of uterine chamber to make into normal shape. With the surgery, implantation of embryo and further development is possible.
- PCO Drilling: Polycystic ovarian can cause the female body produce excess of testosterone and insulin, leading to fertility problems. High testosterone levels can cause irregular menstrual cycles, prevent ovulation and hinder pregnancy. Ovarian drilling can cure this problem Ovarian drilling is a laparoscopic procedure performed under general anesthesia. This surgery is typically done on an outpatient basis with minimal recovery time. With a laparoscopic tool small openings are mad in ovarian.
- Ovarian cystectomy: Endometriomas or chocolate cysts are benign masses growing around ovarian and obliterate the normal process of ovulation. Removal of these cysts is called cystectomy. The surgery needs to be done very carefully as there is a possibility of damage to ovarian vascular supply. Further, there is some decline in ovarian functioning after surgery. So, ART may be necessary for pregnancy.
Male:
- Treat varicocele(swelling of veins coming of Testis) which will allow testes to produce better sperms.
- Removal of blockage in the Epididymis (tubular extension of testis responsible for activation of spermatozoa).
- Reversal of Vasectomy. This is done when the couple decides to go for pregnancy after vasectomy surgery.
- Removal of sperms from testis surgically in case of Azoospermia (Absence of sperms in Ejaculate).
Microbiome Investigation
What is it?
The results demonstrated existence of an endometrial microbiota that is highly stable during acquisition of endometrial receptivity. However, poor reproductive outcomes for in vitro fertilization patients is associated with pathological modification of its profile. This finding provides a novel microbiological dimension to the reproductive process.
How is it done?
Endometrial fluid and vaginal aspirate are investigated for studying the microbial composition. On the basis of these findings distinction was made as a Lactobacillus-dominated microbiota (>90% Lactobacillus spp.) or a non-Lactobacillus-dominated microbiota (<90% Lactobacillus spp.). Although the endometrial microbiota is not regulated hormonally during the acquisition of endometrial receptivity, the presence of a non-Lactobacillus-dominated microbiota in a receptive endometrium was associated with significant decreases in implantation [60.7% vs 23.1% (P = .02)], pregnancy [70.6% vs 33.3% (P = .03)], ongoing pregnancy [58.8% vs 13.3% (P = .02)], and live birth [58.8% vs 6.7% (P = .002)] rates.
When is it recommended?
Uterocervical microbial colonization has been suspected to influence conception rates, with possible causes including an association between cervical microbial species and a pre-existing uterine infection, or colonization of the endometrium or the embryo during transport through the colonized cervix. This kind of microbiota has a significant impact on reproductive outcome even in ART procedures. So, ART failure for no known reason makes it mandatory to examine the Uterocervical microbiota so as to eliminate this as possible reason for ART failures. Thus, the main purpose is to investigate the impact of vaginal microbiome composition on reproductive outcomes within the context of infertility treatments, and the implications this have on assisted reproductive technology procedures.
PGD - Pre-implantation Genetic Diagnosis
What is it?
Pre-implantation Genetic Diagnosis is genetic screening technique which allows an expert to examine the genetic composition of a pre-embryo before it is transferred to the patient’s uterus so that, transmission of hereditary disorders into next generation can be avoided.
Why is it recommended?
A normal human genetic code consists of 23 pairs of chromosomes, and each of the chromosomes may contain hundreds of genes. This genetic material is inherited from gametic cells of both mother and father. The combination of these genes creates the character blueprint for the offspring. Unfortunately, the process may not always work seamlessly. Disorders in the chromosomes or particular gene lead to complications in pregnancy or miscarriage or serious genetic diseases. PGD can help in identification of the issues well before the pregnancy occurs.
In an IVF cycle, the embryos are selected using visual criteria: the embryo or embryos that look healthy are chosen for transfer. Sometimes, a visual inspection is not enough. Some serious genetic abnormalities are invisible to the eye. This is where PGD can be used. Following hereditary abnormalities can be identified with PGD:
- Turner’s syndrome.
- Klinefelter’s syndrome.
- Translocation which can cause miscarriages or some forms of leukemia or cancer.
- Cystic fibrosis.
- Tay-Sachs disease.
- Duchenne muscular dystrophy.
- Sickle-cell anemia.
When is it recommended?
PGD can be recommended in following conditions:
- Women age 35 and older because there is a concern about the genetic quality of their eggs.
- Women experiencing recurrent, unexplained pregnancy loss.
- Women with more than one failed fertility treatment.
- Carriers of sex-linked disorders – they can choose gender determination to prevent sex-linked disease.
- Carriers of single gene disorders.
- Couples with family history of inherited disease.
- Those with chromosomal disorders.
What are the advantages?
- Avoids the need for amniocentesis (with a needle and syringe, some amniotic fluid from around the embryo is drawn for pre-natal examination) which be an uncomfortable technique and involves some risk.
- Enables the selection and implantation of healthy pre-embryo resulting into better chances of pregnancy and lower possibility of miscarriage.
- With proper screening fewer embryos are used for transfer thus, minimizing possibility of multiple births.
PGS - Pre-implantation Genetic Screening
What is it?
It is the genetic study of embryo produced during IVF treatment & can help in having a healthy baby. The technique is helpful to identify embryos with the correct number of chromosomes for successful fertility treatment. PGS is performed on the embryo before it is transferred. This allows the identification & transfer of embryos free from any hereditary abnormalities.
When is it recommended?
It is recommended under following conditions:
- If the female partner is more than 35 years.
- The female has suffered 2 or more miscarriages.
- There is history of previous IVF failures.
- Infertility is due to some male factor.
What are the advantages?
- Reduced miscarriage rates.
- Higher pregnancy rate per transfer.
- Greater chances of having a healthy baby.
Blastocyst Transfer
What is it?
The embryo formation after fertilization involves a number of stages such as 2 cell, 4 cells, 8 cells stage, Morula and so on. Gradually, the cells become distinct as outer cells (Trophoblast) and inner cell mass (embryonic cells). There is a small cavity in between. This stage is called blastocyst. Usually, the protective covering of embryo (Zona Pellucida) is still intact. The blastocyst hatches out of this covering to get implanted into endometrial lining (Innermost covering of uterus).
Using this blastocyst (developed in laboratory) for embryo transfer in IVF technique is called blastocyst transfer (Blast transfer).
When is it recommended?
Blast transfer is recommended for those patients with one more of the following conditions.
- The patients of higher age (35 years or more).
- Repeatedly failed IVF cycles.
- Recipient patients (who are receiving eggs or embryos from donor).
- Those who don’t have the mental preparation for further IVF cycles.
What are the advantages?
- Higher success rates even for patients of higher age.
- Growth pattern of the embryo is established in the laboratory before implantation. So, the doctor has a clear understanding about progress of embryo after implantation.
Sperm DNA Fragmentation
What is it?
It is a test performed with fresh ejaculate received from the patient. This is an effective method for measuring DNA damage in thousands of sperm in the ejaculate. It measures the susceptibility of sperm DNA to denaturation process such as exposure to heat or acids. After this exposure sperms are stained with a fluorescent probe (dye) that interacts with the DNA molecule. Then quantitative analysis made about sperms with fragmented DNA.
How is it done?

- Freshly collected ejaculate is subjected to treatment with certain agents like acids or heat.
- The sample is then stained appropriately and observed under microscope to find out the proportion of sperms with fragmented and non-fragmented DNA.
- On the basis of this proportion suitability of the semen sample for IVF, ICSI or IMSI can be decided.
How can it be treated?
- Damage caused to sperms by oxidative stress can be treated with change in lifestyle and appropriate diet for avoiding oxidative stress.
- If the damage is due to infection, treatment of infection with antibiotics can be beneficial in reducing sperm DNA damage.
- Varicocoele is one of the commonly known causes of male infertility and it is associated with sperm DNA damage. Treating varicocoele can improve sperm DNA integrity.
- Generally DNA damage occurs at the post-testicular (i.e. in the ejaculate) level and testicular sperms are likely to have healthier DNA integrity than ejaculated sperms. ICSI may be an effective treatment than IVF for sperm with high DNA fragmentation.
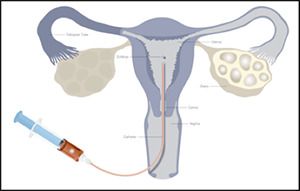
IVF : In Vitro Fertilization
What is it?
During IVF, an egg is removed from the woman’s ovaries and fertilised with sperm in a laboratory. The fertilised egg, called an embryo, is then returned to the woman’s womb to grow and develop. It can be carried out using patient’s eggs and partner’s sperm, or eggs and/or sperm from donors.
When is it recommended?
Offered to women under the age of 43 who have been trying to get pregnant through regular unprotected sex for 2 years, or who have had failed cycles of artificial insemination.
How is it done?
IVF involves 6 main stages:
1. suppressing your natural cycle– the menstrual cycle is suppressed with medication
2. boosting your egg supply– medication is used to encourage the ovaries to produce more eggs than usual
3. monitoring your progress and maturing your eggs– an ultrasound scan is carried out to check the development of the eggs, and medication is used to help them mature
4. collecting the eggs– a needle is inserted into the ovaries, via the vagina, to remove the eggs
5. fertilizing the eggs– the eggs are mixed with the sperm for a few days to allow them to be fertilised
6. transferring the embryo(s)– 1 or 2 fertilised eggs (embryos) are placed into the womb
Once the embryo(s) has been transferred into patient’s womb, she’ll need to wait 2 weeks before taking a pregnancy test to see if the treatment has worked.
Uterine Natural Killer Cells Detections
What is it?
Human immune system is capable of identifying and destroying invading microbes or foreign cells. This mechanism involves participation by certain specialized cells called Lymphocytes. The immunity present right from birth is innate immunity in which Natural Killer Cells play a significant role. These are different from the cells that protect our body from infections. NKCs are able to identify own body cells from foreign cells. During pregnancy the foetus in formation has both maternal and paternal combination of chromosomes and there is possibility of tissue conflict because the growing embryo or foetus is nourished through placenta. Uterine wall releases natural killer cells at the time of pregnancy. These cells some times identify placenta or embryonic cells are foreign cells and are likely to attack them. Usually rate of their synthesis increases during menstruation but diminishes and stops at the time of delivery.
If in their number does not decline, then there is possibility of miscarriage. Corrective measures are required in such conditions.
How is it done?
Either by conducting blood analysis and investigating activation level of the killer cells or by extracting and investigating tissue of uterine wall it is possible to diagnose the problem and suitable treatment like suppressing immune response or prescribing appropriate hormone therapy can overcome this problem.
When is it recommended?
If the patient has a history of repeated miscarriages and investigation reveals the causative factor as Uterine Natural Killer Cells, above said treatment is recommended.
Autoimmune Diseases
What is it?
This is a condition in which the defense mechanism of the body starts identifying normal body cells are foreign cells and starts destroying them. In short, the immune system has been misguided against own body cells and can lead to serious consequences. This kind of disorder can affect endocrines, muscles, digestive system or gonadal organs (Testis or Ovary). Effects on endocrines or gonadal organs can result into infertility. Immunity against ovary minimized the ovarian reserve.
How is it diagnosed?
Autoimmune disease affecting ovary can be diagnosed by checking the ovarian reserve. This is done by analyzing the levels of FSH (Follicle Stimulating Hormone) and AMH (Anti Mullerian Hormone) in blood. Abnormally excess values of these hormone for a particular age could be due to reduced ovarian reserve and is likely to cause early menopause or infertility.
What are various autoimmune diseases?
Thyroid disease: Thyroid gland plays very important role in most of the body activities. Its autoimmunity in women, can reduce the pregnancy rate and can lead to miscarriage.
Anti-sperm Antibodies: Some times in men, antibodies are generated against own sperms. This may reduce the number or motility of sperm and reduce the chances of fertilization in female partner. The men who have had history of testicular trauma or surgery, reversal of vasectomy or treatment for varicocele are likely to have this type of antibodies.
Antiphospholipid Antibody Syndrome: This is a disorder in which antibodies are generated against a particular component of placental tissue resulting into miscarriage, certain pregnancy complication or placental abruption.
How is it treated?
Once diagnosed, the particular disease can be treated with appropriate medication and possibility of conception can be increased. Specific fertility treatment can provide a respite.
Karyotyping
What is it?
Some times, hereditary factors could be responsible for infertility. In such cases before recommending any line of treatment, it is necessary to diagnose the cause of infertility. Studying the genetic or chromosomal composition of the concerned patient to rule out the genetic factor is done in Karyotyping.
PGD (Preimplantation Genetic Diagnosis) involves using one of the embryonic cell for kayotyping. If any defect is detected such embryos can be discarded and healthy embryos can be used for implantation.
Every normal body cell except Red Blood Cells has a set of 46 chromosomes (23 pairs) in its nucleus. These chromosomes are received from both the parents. These can be arranged in 23 pairs out of which the 23rd pair (Sex chromosomes or heterosomes) defines sex of the individual while other 22 pairs (somatic chromosomes or autosomes) of chromosomes define other body characters. Various units of heredity (genes) are located on these chromosomes. In karyotyping technique the integrity of chromosomes can be identified and any aberration in them can be detected. This can give an insight about any congenital abnormality that can result in the child to be born.
How is it done?
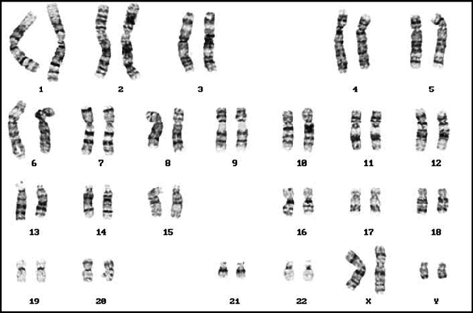
- Venous blood is drawn from concerned patient.
- Cells in the drawn blood are grown in laboratory and are allowed to grow.
- These cells are then stained appropriately and observed under microscope.
- By a specialized technique, it is possible to observe chromosomes from these cells and thus, genetic disorder if any can be diagnosed.
When is it recommended?
Karyotyping is recommended under following conditions so as to define the genetic anomaly and prevent it from being passed on to next generation.
- If the patient is not able to conceive for over year.
- There is a history of still births.
- Miscarriages are reported.
- Primary ovarian dysfunctions such as Primary ovarian insufficiency (POI), Premature Ovarian Failure (POF) are diagnosed as reasons for infertility in female partner.
- Infertility in male partner is found to be due to very few sperms in semen (Oligozoospermea) or absence of sperms in semen (Azoospermea).
What are the advantages?
- If cause of miscarriages is found to be genetic in origin, suitable treatment can be recommended to overcome it.
- By identifying defective genes in the parents, their being into next generation can be avoided.
- There are certain disease-causing genes either of the parents can be carrying. Some of these may be found in both the parents and can result into serious consequences if passed on to the next generation. This can be avoided by carrying out karyotyping of parents. Cystic fibrosis is one such example.
In routine IVF technique, usually a healthy sperm participates in fertilization but, if ICSI is carried out even an unhealthy sperm can be used for fertilization.
Fertility Booster Diet
Intake of proper food becomes very important during the fertility treatment. Eating certain foods during different phases of your menstrual cycle can enhance the fertility. So, if a woman wants to maximize her chances of conceiving, it is possible to eat foods that have advantageous to each phase. So, we ask our experts to weigh in on what to actually eat during each of the reproductive phase.
The list includes:
1. Plenty of fruits and vegetables
2. Complex carbohydrates – whole grains like brown rice , oats and whole meal bread .
3. Organic food where possible.
4. Oily foods like nuts, fish and oil.
5. Add lemon , pomegranate, green leafy vegetables and tomatoes to diet .
6. Flax seeds + sunflower seeds .
7. Avoid trans fats.
8. Increase intake of fibre.
9. More fish and organic eggs than red meat .
10. Avoid additive ,preservatives and artificial sweetner.
11. Reduce and avoid sugar both on its own and hidden in food .
12. Avoid caffeine : coffee, chocolate ,tea ,cola & alcohol .
13. Avoid processed food.
14. Try having fresh and home-made food.
Weight Loss Management
What is it?
It is avoiding weight gain or losing weight for improving the chances of conceiving. Too low or too high body weight can interfere with fertility of an individual and hence, needs to be managed appropriately.
How is it done?
Normally, weight loss management involved diet and exercise. The couple trying for pregnancy needs to take careful measures in this. Proper diet and moderate exercise are best recommended for weight loss. But during pregnancy if necessary, weight management must be done preferably by diet control. Heavy exercise can affect the embryonic development in uterus and hence, has to be avoided.
When is it recommended?
Excess body weight in female partner is known to reduce the possibility or pregnancy. There is a need to manage the weight appropriately for natural pregnancy or even IVF. When an obese patient approaches for IVF treatment, before treatment the patient needs to undergo weight management regime and only then the IVF protocol can be followed. As mentioned above, the weight loss should be by controlled diet and not entirely by exercise.
Immunotherapy for Pregnancy
What is it?
Sometimes, female partner’s blood identifies lymphocytes from male partner as immunogens and reacts to them. In such cases, an aspect of immune-compatibility occurs leading to difficulty in conceiving. Active Immunotherapy can be an appropriate solution in such patients wherein, this type of immunity is suppressed and then ART can be tried.
When is it recommended?
Recurring miscarriages in a patient could be due to immune response by female partners blood to male partner’s lymphocytes. In such cases, after confirming cause of miscarriages as immune response immunotherapy can be recommended.
How is it done?
The blood from concerned patient is drawn and tested for confirming its reaction with male partner’s blood sample. If the cause is identified as immunity, immunotherapy is started.
- Some blood is drawn from female partner’s body and plasma is separated from it. Male partner’s lymphocytes are suspended in it.
- This plasma is then injected into female partner. The treatment involves injecting it in different doses as intravenous, intradermal and subcutaneous doses.
- The IVF or normal conception can happen 4-6 weeks after the treatment.
What are the advantages?
- If the root cause of miscarriages is immune response, this treatment can eliminate this cause.
- Success rate of this treatment has been observed to remarkably high.
- Though the cost of treatment increase, it is worth trying due to its success rate.
